Lower Leg Injury Resource Center
Plantar Fasciitis
Causes, Diagnosis and Treatment

Plantar fasciitis is a common condition which affects the bottom of your foot. The most common symptom is pain around your heel and arch, especially first thing in the morning. It can usually be treated at home, but recovery can take several months.
This article covers the main symptoms and causes of plantar fasciitis, treatment options and recovery time, and answers the most frequently asked questions about the condition.
I
WHAT IS PLANTAR FASCIITIS?
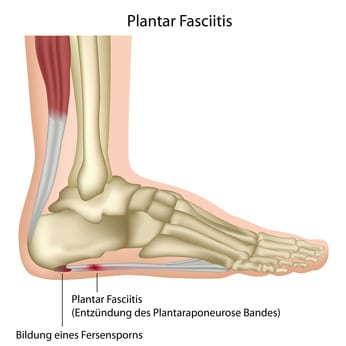
Plantar fasciitis is a condition caused by the thick band of tissue that extends from your heel to your toes becoming inflamed. This ligament, which is called the plantar fascia, acts as a shock absorber and supports the arch of your foot as you walk. Most of the time it can handle the everyday stress and strain that we put on our feet, but occasionally it becomes irritated and inflamed, causing pain and discomfort.
Plantar fasciitis is a common condition and affects around one in 10 people[1]. With the correct treatment, around 80% of cases improve within 12 months and it doesn’t usually require surgery. However, it can be painful to live with and interfere with your normal day to day life, so it’s important to treat it as soon as possible.
I
CAUSES OF PLANTAR FASCIITIS
It’s not always clear what causes plantar fasciitis. However, there are some factors which are thought to increase the likelihood of developing this condition. They are as seen below:
- High impact sports like running, tennis, dance etc
- New or increased activity over a short period of time
- Exercising on hard surfaces
- Jobs that require you to be on your feet for much of the day
- Having a tight Achilles tendon or calf muscles
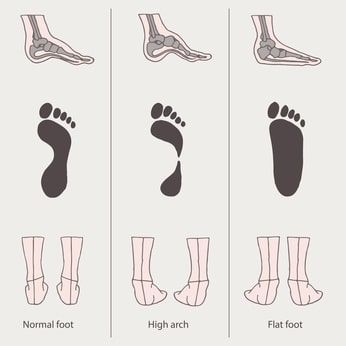
- High arches or flat feet
- Poor fitting footwear which doesn’t provide enough cushioning or support
- Age – it’s more common between the ages of 40 and 60
- Obesity

I
SYMPTOMS OF PLANTAR FASCIITIS
The most common symptom of plantar fasciitis is pain. This is typically described as a stabbing sensation at the bottom of your foot near your heel, which is worse in the morning when you take your first steps and may subside as you continue to walk. The pain may get worse as the day progresses. It may flare up again after exercise, long periods of standing or when you get up after sitting for a while.
Symptoms of plantar fasciitis can come and go so it can be easy to ignore the signs at first and just carry on as usual. But if left untreated, the condition is likely to get worse.

I
DIAGNOSING PLANTAR FASCIITIS
You can usually diagnose plantar fasciitis at home from your symptoms. You can also try this simple exercise, which tests how tender the area is:
- Using your hand on the same side as the injured foot gently pull your toes back, towards your shin.
- With your other hand, use your fingers to tap the sole of your foot, approximately 1-2 inches in front of your heel.
- If it feels painful, you probably have plantar fasciitis.
If your symptoms don’t improve after a couple of weeks, it’s best to see your doctor. They will examine your foot to see how tender it is and may order an X-ray to rule out other causes of heel pain, such as stress fractures or bone spurs.
I
TREATMENT FOR PLANTAR FASCIITIS
Most cases of plantar fasciitis don’t require surgery and can be treated at home. However, it can take up to a year to make a full recovery so it’s important to prepare yourself mentally and not to rush things, no matter how frustrating it can be. Here are some main treatment options:
Rest
If the pain gets worse after certain activities, you’ll need to decrease or stop them completely to give the inflamed tissue a chance to recover.
Ice
Roll your foot over a frozen water bottle or use ice for 20 minutes to reduce inflammation up to four times a day. Remember not to apply ice directly on to your skin.
Medication
Over the counter medication like ibuprofen (eg Advil, Motrin IB) and naproxen sodium (Aleve) may help to ease pain and inflammation.
There are some other things that you can do to help your recovery:
Wear Proper Footwear
Make sure that your shoes are well-fitting, comfortable and supportive. Not only will this aid your recovery but it could help to prevent plantar fasciitis in the future.
No one size fits all so it’s important to know your foot type before choosing your footwear. If you have high arches, make sure you get shoes that fill in and support the arch. If you have flat feet, you need shoes that build up your arch. You can buy soft silicone heel pads from drugstores which can help to elevate and cushion your heel. Avoid high heels and flats as much as possible – a small heel is best. In some cases, orthotics can be helpful.
Exercise
Tight muscles in your feet and calves can aggravate plantar fasciitis. Stretching is the most effective way to relieve the pain associated with this condition. Try the following:
Toe stretches
Sit in a chair and pull your big toe towards your ankle gently but firmly. Hold for 30-45 seconds then repeat with each toe. Do this 2-4 times a day.
Calf Stretches
Place your hands on a wall with your palms open for support, then move your affected leg back until you feel a comfortable tension in the center of your foot. With your heel planted firmly down, move your knee forward slowly and gradually for 2 minutes. Repeat 1-2 times daily.
Towel or Band stretches
Sitting on the floor with your legs flat on the ground, wrap a towel around the ball of your foot then pull gently for around 30 seconds. Repeat 2-4 times daily.
Arch stretches
Place a rubber roller under your foot and roll forward and back for several minutes. Repeat a few times throughout the day.
Cortisone Injections
Cortisone is a powerful anti-inflammatory and can be injected directly into the plantar fascia ligament to reduce inflammation and pain. However, it’s important not to have too many cortisone injections because they can lead to rupture of the fascia, flat feet and chronic pain.
Night Splints
Most of us tend to sleep with our feet pointed down. Wearing a night splint will keep your foot at a 90-degree angle, stretching it while you sleep. Night splints can help to alleviate your pain and as soon as you feel better you can stop using them.
Physical Therapy
A physical therapist can give you an exercise programme to stretch your calf muscles and plantar fascia. They may also use ice treatments, massage, ultrasound, and medication to reduce inflammation.
Extracorporeal Shockwave Therapy
This procedure uses shockwaves to stimulate healing in the plantar fascia tissue. The shockwaves work by increasing blood flow to the injured area and speeding up the healing process. Opinion is mixed on how effective this method is, but some studies have found[2] that it can be an effective treatment for people with plantar fasciitis.
I
SURGICAL TREATMENT FOR PLANTAR FASCIITIS
Occasionally nonsurgical treatments don’t work, and your doctor may suggest surgery. This is usually seen as a last resort when all other options have failed after six to 12 months of trying. Around 5 in every 100 patients with plantar fasciitis will need surgery.
The most common surgery is plantar fascial release. During the procedure, the surgeon will cut part of the plantar fascia ligament to release the tension and relieve swelling. This is usually done as open surgery, where a 3cm incision is made around the heel pad. If you have any bone spurs, these will be removed too. It may also be done endoscopically, using instruments fed through tiny incisions in your foot.
However, a surgery called Gastrocnemius Recession may be used instead. This is where one of the two muscles that make up the calf is lengthened to increase motion in the ankle. Again, this can be done as open or endoscopic surgery. Evidence suggests[3] that this procedure can improve function and outcome for people with plantar fasciitis.
The most common complications of surgery are nerve damage and failure to fully relieve the pain. However, the majority of patients have good results.
Recovering from Plantar Fasciitis Surgery
It takes around six weeks to recover from surgery. During this time, you will need to be non-weight bearing, which means keeping the weight off your injured foot completely. This can be a frustrating time but fortunately there are now some great alternatives to crutches that you can use during your recovery to keep you mobile and active.
Here are your main options:
Traditional Crutches
Traditional crutches are easy and cheap to get hold of and are often the first thing people try after surgery. However, they can be exhausting to use and can cause additional pain in other parts of your body, particularly your arms and hands. They are also restrictive because you can’t carry anything, which prevents you from carrying out normal day to day activities.

Knee Scooters or Knee Walkers
Knee scooters or “knee walkers” are another option. They are more efficient than crutches and require less upper body strength. However, they are still quite restrictive as they can’t be used on stairs, slopes or uneven terrain. They also require the use of your hands to operate the scooter and they are bulky, which makes them difficult to transport.

iWALK Hands-Free Crutch
The iWALK is a hands-free and pain-free crutch that enables you to walk around unaided with full use of your hands and arms. You kneel on a padded platform with your injured leg elevated and secure, and the device becomes a temporary prosthetic lower leg. The iWALK crutch allows you to get back to your daily activities while you recover and it can be used on stairs, slopes, uneven terrain and in the shower. A 2019 medical study[4] found that nine out of 10 patients prefer the iWALK crutch to traditional crutches.

I
TIPS FOR PREVENTING PLANTAR FASCIITIS
Unfortunately you can’t completely prevent plantar fasciitis but there are some things that you can do to help reduce the risk:
- Stretch regularly (see the exercises suggested above)
- Wear suitable, well-fitting footwear
- Learn to relax your lower legs
- Land evenly in the middle of your foot when walking and running
- Avoid uneven surfaces when running
- Indulge! Foot massages can help to keep the plantar fascia loose
I
FAQ
Here are the most commonly asked questions about plantar fasciitis:
Do you need crutches for plantar fasciitis?
Most people won’t need to use crutches for plantar fasciitis. However, in severe cases you may need to rest your foot completely which means you’ll need crutches, a knee scooter or the iWALK hands-free crutch. If you have surgery, you’ll be non-weight bearing for around six weeks and during this time you’ll need to use a mobility device too.
How long after plantar fasciitis surgery can I walk?
The recovery time for plantar fasciitis surgery is six weeks. During this time, you will probably need to keep the weight off your foot completely. Your doctor will tell you when you can start to bear weight again. It can take several months to make a full recovery.
How long does it take for plantar fasciitis to heal?
In most cases, plantar fasciitis gets better with the correct treatment but it can take up to a year. Once you’ve had it, you’re more likely to get it again. Our tips for preventing plantar fasciitis (above) can help to reduce the risk of this happening.
What is the best treatment for plantar fasciitis?
Most cases of plantar fasciitis can be successfully treated with rest, ice, and over the counter pain medication. Stretching exercises can also help with recovery. However, other treatments like cortisone injections, shockwave therapy and night splints have been used. Only 5% of people with the condition will need surgery.
What are the best shoes for plantar fasciitis?
Your shoes should be well-fitting with ample arch support and a firm, but flexible midsole. Make sure there is plenty of cushioning in the forefoot. You can also buy silicone heel pads from drugstores which you can insert into shoes. Shoes with a small heel are your best option – both high heels and flats can aggravate the problem.
The information above is intended for informational purposes only and is not intended to prevent, treat, or diagnose any illness or disease. We aim to provide the highest quality information, so if you have any questions on the information above, we welcome your feedback!
I
RESOURCES
- https://www.aafp.org/afp/2019/0615/p744.html
- https://www.ncbi.nlm.nih.gov/pubmed/31435724
- https://www.podiatrytoday.com/closer-look-gastroc-recession-recalcitrant-plantar-fasciitis
- https://www.ncbi.nlm.nih.gov/pubmed/31375043