Lower Leg Injury Resource Center
Achilles Tendon Rupture
Symptoms, Causes, Treatments, Surgery and Recovery

Kevin D. Martin, DO, FAAOS
Orthopedic Foot and Ankle Surgeon
Associate Professor of Surgery
About the author – Dr. Martin specializes in orthopaedic surgery of the foot and ankle. In addition to his practice Dr. Martin serves as committee member of the American Orthopaedic Foot and Ankle Society and is a regular contributor to multiple medical journals including Foot and Ankle International.
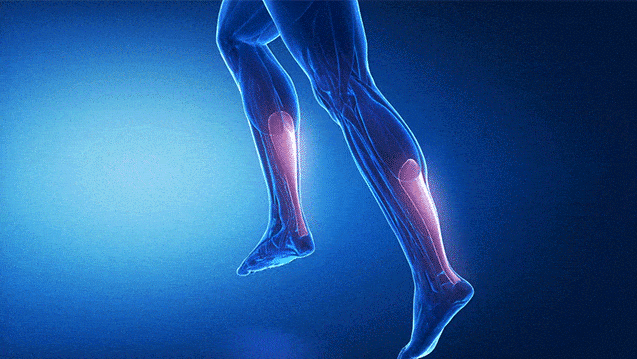
The Achilles is a commonly injured tendon. Many Achilles tendon injuries are caused by overuse, which leads to a swollen and painful tendinitis. In the most severe Achilles tendon injuries, too much force on the tendon can cause a partial tendon tear. In the worst cases, a complete Achilles tendon rupture results [1].
There is a wide range of symptoms [2] that you may experience when you injure your Achilles tendon, from a weakness in your leg, to hearing an audible pop followed by leg pain. Whether you already have an Achilles tendon rupture diagnosis or are experiencing symptoms, there are many questions to answer.
Achilles Tendon Rupture
Table of Contents
I
CAUSES OF AN ACHILLES TENDON INJURY
The Achilles tendon does a massive job and can usually withstand great stress from running, jumping and a wide range of daily activity. The Achilles is also prone, however, to tendinitis, which is an inflammation of the tendon, and rupture, a condition associated with overuse or degeneration [4].
In an Achilles rupture, the Achilles tendon itself tears, either partially or completely. This can happen due to degeneration over time or can happen abruptly from an acute injury.
Achilles injuries occur most often when pushing with sudden force off the foot, as with jumping or sprinting. This is common in sport-related injuries like running, dance, tennis, volleyball, football, basketball, baseball and other sports that require a lot of quick stops and starts.
There are many reasons an Achilles tendon can weaken or get injured [5]. Taking certain medications, wearing high heels and overuse can contribute, as can underlying disease, age and arch issues. Additionally, a sudden increase in physical activity and lack of stretching are other common factors that can lead to an Achilles tendon injury.
I
SYMPTOMS & DIAGNOSIS OF A RUPTURED ACHILLES TENDON
Common symptoms of an Achilles tendon rupture include:
- A snap, crack or popping sound when pushing off with your leg
- A sharp pain in the back of your leg or ankle
- Trouble moving your foot to walk or climb stairs
- Inability to stand on your toes
- Pain, bruising and swelling at the back of your leg or heel [6]
If you have any of the above symptoms, seek immediate medical attention for a complete diagnosis of your Achilles tendon.

I
PARTIAL TEAR VS COMPLETE RUPTURE
There are a number of observations and tests your physician will perform to determine the extent of your Achilles tendon injury, including visual observation and possible image testing such as an MRI or ultra sound. They may also perform a physical exam called the Thompson test.
The Thompson test is a physical exam that’s performed with the patient on their stomach and their knee bent. The physician squeezes the calf to see if the foot moves toward the ceiling. If the foot does not move, the Achilles tendon is torn or ruptured.
Partial Achilles Tear
If the tear is partial you may still be able to walk, but you will have a limp, often accompanied by severe pain when you push with your toes or touch down on your heel.
In addition, the middle section of your Achilles will be tender and swollen, a symptom that will likely subside after a few days.
Your Achilles tendon may also be painful and stiff, especially after a long period of inactivity [7].
Complete Achilles Tear / Achilles Tendon Rupture
More severe than a partial tear, a total Achilles rupture will be more obvious [8], and you will likely notice the moment the injury occurs. Symptoms may include:
- Acute pain, often described as being struck by a sharp object in the Achilles area
- A loud snap or pop that can be heard at the time of injury
- Difficulty flexing and pointing your foot
- Formation of a small visible gap or palpable depression in back of the calf.
If any of these symptoms are present, it’s highly likely you have an Achilles rupture, and you should immediately have your injury assessed and verified by a physician to avoid more damage and give yourself the best chance for a full recovery.
Note that a partial Achilles tear is not as easy to diagnose as a complete Achilles rupture, and you might not notice when the injury occurs. Partial tears often don’t reveal themselves until after you cool down from your activity.
I
MANAGING ACHILLES TENDON PAIN & INFLAMMATION
If you have any of the above symptoms and cannot see a doctor immediately, you can treat your rupture at home for a short time. However, Achilles tendon injuries should not be taken lightly because you can inadvertently cause additional damage. It’s important to see your physician as soon as possible to learn more about Achilles Tendon repair [9].
Start With Ice to Reduce Inflammation
Placing ice on the most painful area of the Achilles tendon is helpful to reduce swelling due to inflammation. Use a piece of thin material between the ice and your skin to protect from ice burn.
You can ice the injury for up to 20 minutes three to four times a day, but make sure to pay attention to the skin. If it becomes red or numb reduce the time and/or frequency of the ice therapy.
Get plenty of rest in conjunction with the ice treatment. It’s best not to walk or stretch a ruptured Achilles tendon, especially if you have extreme pain.

Medications for Inflammation and Pain
You may want to take a pain-relief medicine to help with the initial discomfort of an Achilles tendon rupture.
Many over-the-counter medications [10] are used not only for pain relief, but also to reduce inflammation. Common over-the-counter pain relievers such as non-steroidal anti-inflammatory drugs (NSAIDs) and aspirin will reduce inflammation.
Your doctor may recommend the following:
- Ibuprofen (Advil and Motrin)
- Naproxen (Aleve)
- Tylenol (Acetaminophen)
- Generic Aspirin
- Topical Creams
It’s important to follow pharmacist and physician instructions regarding use of any medication. Improper or overuse of over-the- counter medicine can lead to more serious damage to the body and internal organs. Allergies should also be considered for any medication.
I
SURGICAL VS NON-SURGICAL ACHILLES TREATMENT
Achilles Injury Non-Surgical Treatment
Once your physician has diagnosed an Achilles injury, whether partial or full Achilles tendon rupture, you may be presented with treatment options [11]:
- Wearing a cast or removable boot that points the toes down.
- Wearing a heel wedge or series of casts that adjust the amount of stretch in your Achilles tendon over time. Using this method, called recasting, a new cast or heel wedge is added weekly to gradually decrease the amount of flexion (toes pointing down) in your ankle. This allows the Achilles tendon to heal while gradually increasing the stretch in the tendon.
While non-surgical procedures can be attractive, recovery rates are not encouraging. Non-operative care has demonstrated a re-rupture rate of 10 to 30 percent while surgical re-rupture rates are around 3 to 4 percent. It is best to consider all options for ruptured Achilles tendon treatment.

Achilles Injury Surgical Treatment
There are two primary types of surgery for Achilles tendon repair. The traditional method involves an open surgery, and the newer method uses a specially-designed device to put the tendon in place while making a smaller incision.
Open Achilles Tendon Tear Surgery
Open Achilles surgery involves a single large incision on the back of the leg, removal of damaged tissue and suturing the ends of the tendon back together.
This type of repair may be strengthened using a tendon transfer from your big toe or from a cadaver and sewing it into the remaining portion of your own Achilles tendon.
Mini-Open Surgery
Mini Open surgeries involve small incisions and small instruments to perform repairs. With an Achilles rupture the technique is called Percutaneous Achilles Repair System (PARS). In this surgery the damaged tendon is repaired without disrupting blood supply while minimizing scar-tissue.
How The PARS Surgery works
The PARS procedure creates a 2-centimeter horizontal incision about 4 to 6 centimeters above the heel to insert the specially-designed PARS device up toward the knee. The PARS device has four prongs, two that go inside the leg to hold the tendon in place and two that go outside the leg.
All four prongs have eight small holes that allow the surgeon to place sutures throughout the tendon including in portions of healthy, non-injured tendon.
This is done because the Achilles tendon doesn’t just snap or tear evenly. Rather, it shreds so that the ends appear similar to a mop head. This makes it essential to suture the whole tendon to facilitate the strongest repair.
Once the top of the tendon is secure the surgeon will pull the threads tight and secure the two ends of the tendon together. Held in this position, the Achilles tendon will mend and heal.
The PARS procedure is not for everyone. The tendon may rupture in a position the device cannot reach, or in cases where the injury is more than seven to 10 days old the tendon rupture may have already begun to heal, making its use difficult or impossible.

“The best treatment for a ruptured Achilles tendon in an active individual is typically surgery. While an Achilles rupture can sometimes be treated with a cast, splint, brace, or other device that will keep your lower leg from moving, surgery provides less chance that the tendon will rupture again and offers more strength and a shorter recovery period.”
– Dr. Sam Labib, Director of Foot and Ankle Service, Emory University
Since Achilles ruptures are so common, surgeons are constantly developing new and innovative procedures for repairing Achilles tendon ruptures. Check with your local orthopedic foot and ankle surgeon to learn about the newest developments and range of options.
Risks of Achilles Tendon Surgery
While Achilles tendon tear surgery produces a majority of positive outcomes, it is not without risks [12], which you should factor into your decision about which Achilles tendon repair to choose. Surgical risks from Achilles tendon rupture surgery include:
- Skin infection at the incision site
- Normal complications of surgery and anesthesia
- Possible nerve damage
- Risk of a repeat Achilles rupture (3 to 4 percent for surgical repair and 10 to 30 percent for nonsurgical treatment)
- Loss of strength in the healed tendon
- Decrease in the range of motion of your Achilles tendon. (Rehabilitation is very important to restore full range of motion.)
I
TORN ACHILLES RECOVERY TIME
After any type of Achilles tendon tear surgery, you will likely wear a cast or walking boot, for six to 12 weeks.
At first, the cast or boot will keep your toes pointed downward as the tendon heals. The angle will gradually be adjusted over time until your foot is in a neutral position, a phase of your recovery when you can’t put any weight on your injured foot at all.
Choosing the right mobility device will help you stay off your injured leg and improve your chances for a full recovery.
Traditional Crutches
Traditional crutches will facilitate getting around without putting weight on your injured leg. They are inexpensive and readily available, but conventional crutches have several disadvantages over contemporary options. Pain is the number one complaint from conventional crutch users. Wrist, hand and elbow pain are common, as is under-arm chafing.
Common activities like walking through a door, pushing a shopping cart, going to work, and cooking in your kitchen are difficult or impossible on traditional crutches, and that leads to widespread cheating when people momentarily put weight on their injured legs. This can cause re-injury or a prolonged recovery.
Because of conventional crutch limitations, patients often begin walking on an injury too soon, which can complicate healing.

Knee Scooters or Knee Walkers
Knee scooters, also called knee walkers, are common and increasingly popular. The user of a knee scooter bends their injured leg 90 degrees at the knee and kneels on a platform that’s attached to frame with wheels. The user steers the knee scooter with handlebars, much like a bicycle or children’s toy scooter.
For long distance mobility, knee scooters are a big improvement over crutches, but they have some significant disadvantages. With a knee scooter, both hands are required to control the device, so scooters restrict numerous daily activities. Even something simple as going through a door can create a challenge.
Getting into a car requires that the heavy and bulky device is stowed in the trunk or back seat, which then requires the user to hop around the car. This can lead to dangerous falls. The turning radius of knee scooters is also limited, so trying to navigate restricted areas, such as kitchens, is challenging.
You cannot use knee scooters on stairs, in small areas, on slopes, or uneven terrain.

iWALK Hands-Free Crutch
The iWALK hands-free crutch is the most cutting-edge mobility device to enter the market. As with the knee scooter, you kneel on a padded platform, but with its straps properly secured, the iWALK becomes an extension of your leg, functioning like your own leg would.
Because your upper leg is performing the same muscle memory routine of walking, learning and using the iWALK hands-free crutch is easy and intuitive. Unlike the knee scooter or conventional crutches, your hands and arms are free to perform normal day-to-day tasks, so walking through a door, pushing a shopping cart, doing laundry and walking your dog are all routine. Even stairs are possible, plus your hands are free to hold the rail.
Recent clinical research showed that 86 percent of non-weight bearing patients preferred the hands-free crutch over other mobility devices [13]. Moreover, new medical studies show the iWALK boosts blood-flow, reduces muscle atrophy and may accelerate healing [14].

Compare the iWALK crutch to other Mobility Devices
I
PHYSICAL THERAPY FAQ
Physical therapy will be an important part of your Achilles rupture recovery whether you had surgery or not. With most injuries, the harder you work on your physical therapy, the better and faster you’ll recover, but that’s not necessarily the case with a ruptured Achilles tendon.
Your Achilles tendon needs time to heal properly. It’s the biggest tendon in your body so giving it time to heal correctly is very important.

Common Questions Regarding Therapy
What will therapy consist of?
Depending on your injury, physical therapy may include deep massage, ultrasound heat therapy, stretching and/or strengthening. These treatments improve blood flow to the area to enhance healing [15].
Strengthening exercises will be introduced at the appropriate stage to get your Achilles back to normal use while avoiding future injury.
How long will I need Achilles tendon physical therapy?
This is a common question that depends on the severity of your Achilles tendon injury. The type of treatment you received and a review of your medical history are also considerable factors. The duration of therapy varies from person to person and hinges in large part on your dedication to the therapy given.
Unfortunately, some people never restore their abilities in competitive sports or running after an Achilles tendon rupture repair. It will typically be four to six months before you can run. It may also take 12 months before you are pain free [16].
Will Achilles tendon physical therapy hurt?
Pain thresholds vary from person to person and also depend upon type of treatment and severity of injury.
Some of the strengthening exercises, which involve tightening of muscles, can cause discomfort, but they’re bearable for most individuals. These exercises done incorrectly can cause damage to the repaired Achilles, so it’s highly recommended that they’re performed under a physical therapist’s supervision [17].
Do I need a physical therapist for Achilles rupture recovery?
A physical therapist will serve as an educator as well as the person who administers treatments like massage and ultrasound heat therapy. They will teach you how to stretch, care, and strengthen your injury as part of Achilles tendon rupture treatment.
The physical therapist’s goal is to relieve pain and inflammation, improve circulation to your Achilles tendon and gradually get you back to normal. A physical therapist offers invaluable support as they design a program tailored to your injury, treatment, activities and fitness level.
Strengthening of the tendon and associated leg muscles doesn’t happen until the very end of the healing process. This means it will take a long time to get back to your pre-injury abilities. Ruptured Achilles tendon treatment can be a long road. Temper your expectations in advance so that you don’t overdo it, and follow your therapist’s instructions.
I
TIPS FOR STAYING POSITIVE & ACTIVE
There’s an emotional side to having a physical injury. Having our bodies damaged and restricting our activities can have a pronounced effect on our emotional well-being.
An Achilles tendon injury can be very limiting and cause you to lose your independence. The severity of the emotional fallout varies from person to person, and frustration and boredom are common side effects. Depression can also result [18].
Maintaining a positive outlook is an important component of your Achilles tendon injury recovery. It’s essential that you go about life as normally as your injury allows. Using a mobility device like the iWALK hands-free crutch will enable you to continue working and taking care of your family during recovery. Knowing you can be independent can significantly lift your spirits.
It’s important to maintain a fulfilling life as you recover, so perhaps this is a good time to start a new hobby you’ve been putting off. Keeping a positive attitude will insure that you are ready to work hard when the time comes to rehabilitate your tendon and get back into the game of life.
I
NUTRITION TIPS TO HELP RECOVERY
Water: Dehydration causes muscle tightness, hydration helps optimize muscle function and rehabilitation.
Pineapples: Bromelain, an enzyme found in pineapples, helps reduce inflammation from injury.
Dairy: It’s time to actually listen to your mom, and drink that glass of milk! The calcium found in dairy such as milk and yogurt is not just good for your bones; it’s good for rebuilding your torn Achilles tendon, too.
Nuts: Almonds, soy beans, peanuts (and peanut butter) all contain calcium and magnesium, which help kick-start the healing process of re-building your injured tendon’s connective tissue. This tip will not work for everyone, as food allergies to nuts are common.
Vitamin C: This well-known vitamin helps repair torn tissue and produces collagen. Collagen is a key protein your body needs to build tendons and ligaments and heal skin. Oranges, bell peppers and strawberries are just some of your options to meet the daily recommended dose [19].
Listen to Your Body
Achilles tendon injuries are common, but they can have a major effect on your life. It’s important to stay in good shape and listen to your body. If you have heel pain, calf pain or swelling on the back of your leg, cut back on your activities, ice and rest your leg. If the problem doesn’t resolve make sure to see your doctor.
The information above is intended for informational purposes only and is not intended to prevent, treat, or diagnose any illness or disease. We aim to provide the highest quality information, so if you have any questions on the information above, we welcome your feedback!
I
RESOURCES
- Picture of the Achilles Tendon. Matthew Hoffman, MD. Jump Start by Web MD. 19 May 2019. https://www.webmd.com/fitness-exercise/picture-of-the-achilles-tendon#1
- Achilles Tendon Rupture. Mayo Clinic. 31 July 2020. https://www.mayoclinic.org/diseases-conditions/achilles-tendon-rupture/symptoms-causes/syc-20353234
- Picture of the Achilles Tendon. Matthew Hoffman, MD. Jump Start by Web MD. 19 May 2019. https://www.webmd.com/fitness-exercise/picture-of-the-achilles-tendon#1
- Tendonitis. Harvard Health Publishing. Harvard Medical School. Accessed 4 June 2021. https://www.health.harvard.edu/diseases-and-conditions/tendonitis
- Achilles Tendon Injuries. Jump Start by Web MD. 21 August 2020. https://www.webmd.com/fitness-exercise/guide/achilles-tendon-injury#1
- Achilles Tendon Injuries. Jump Start by Web MD. 21 August 2020. https://www.webmd.com/fitness-exercise/guide/achilles-tendon-injury#1
- Achilles Tendon Tear. Standford Health Care. Accessed 4 June 2021. https://stanfordhealthcare.org/medical-conditions/bones-joints-and-muscles/achilles-tendon-tear.html
- Achilles Tendon Rupture. Christopher C Nannini, MD. emedicinehealth. 31 January, 2020. https://www.emedicinehealth.com/achilles_tendon_rupture/article_em.htm
- 1 June 2011. https://www.hss.edu/conditions_chronic-achilles-tendon-problems-overview.asp
- Achilles Tendonitis. Mayo Clinic. 17 September 2019. https://www.mayoclinic.org/diseases-conditions/achilles-tendinitis/diagnosis-treatment/drc-20369025
- Achilles Tendon Injuries. Web MD. 21 August 2020. https://www.webmd.com/fitness-exercise/guide/achilles-tendon-injury#1
- What is Achilles Repair Surgery? Johns Hopkins Medicine. Accessed 7 June, 2021. https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/achilles-tendon-repair-surgery
- Martin KD, Unangst AM, Huh J, Chisholm J. Patient Preference and Physical Demand for Hands-Free Single Crutch vs Standard Axillary Crutches in Foot and Ankle Patients. Foot Ankle Int. 2019 Oct; 40(10):1203-1208. https://journals.sagepub.com/doi/full/10.1177/1071100719862743
- Comparison of Lower Extremity EMG Muscle Testing With Hands-Free Single Crutch vs Standard Axillary Crutches. Cuyler Dewar, MS, Kevin D. Martin, DO, FAAOS, DAL. Foot and Ankle Orthopaedics. 2 September 2020. https://doi.org/10.1177/2473011420939875
- Achilles Tendon Injury: Physical Therapy and Rehab. Michigan Medicine, University of Michigan. 16 November 2020. https://www.uofmhealth.org/health-library/tr2261
- How to Recover from Achilles Tendon Injury. Jump Start by Web MD. 19 December 2010. https://www.webmd.com/fitness-exercise/recovering-from-achilles-tendon-injury#1
- Exercise Program for Achilles Tendon Rupture. Brett Sears, PT. Verywell Health. 20 July, 2020. https://www.verywellhealth.com/pt-exercises-for-achilles-tendon-tear-4165931
- Chronic Pain and Depression. Kathleen Smith, PhD, LPC. 7 May 2021. https://www.psycom.net/depression.central.chronic.pain.html
- The top 14 Foods and Supplements for Sports Injuries. Alina Petre, MS, RD. Healthline. 14 January 2017. https://www.healthline.com/nutrition/foods-supplements-for-sports-injury